Like a fine wine, we’d hope that most things get better with age, including sex! But once menopause rolls around, it’s not always smooth sailing to navigate the bodily changes and role-shifting that often accompanies this physiologic event. Menopause, happening at midlife or when induced, can feel like a road block that affects libido and the health of the pelvic floor in a negative way. Menopause causes physical changes in the body, and when it occurs at midlife it is also can be intertwined with other illness and life events that happen at the same time. While this sounds like doom and gloom, equipping yourself with the knowledge of what’s going on in the body and what you can do about it can empower you to navigate sex and menopause in a way that feels right for you.
What is menopause?
Menopause marks the the end of the reproductive years. It’s defined as a lack of a menstrual cycle for 12 months, in the absence of other causes, like long-term contraception. Menopause happens naturally for anyone who has a uterus and ovaries, with an average age of onset of 51 in the United States. But it can also be surgically or pharmacologically induced, such as when someone has their ovaries removed during a hysterectomy, or if taking estrogen suppressing drugs, like after breast cancer or with folks taking hormone blockers.
Physical changes in menopause
As ovulation stops, a huge hormonal shift rolls in like a storm, and has several effects on the body. Many of these changes are systemic, but have a local effect on the pelvic floor muscles and the vulvar tissues.
- Estrogen levels drop significantly, similar to what happens during breastfeeding. Estrogen gets labeled as a purely reproductive hormone, but it also plays a role in bone density, cardiac health and autoimmune disorders. As a result, when estrogen dips during menopause, bone density drops, and the incidence of autoimmune and cardiac disorders increases.
- The body loses muscle mass in a process called sarcopenia, and the pelvic floor muscles are not spared from this. In addition to the muscles getting smaller, non-muscular tissue also thins as well, meaning that the labia and other parts of the vulva get thinner.
- Urinary incontinence, leaking urine when you don’t intend to, becomes more common, such as with coughing, sneezing, lifting, or associated with a strong urge. This is partially because the muscles and the tissue around the urethra start to thin, and it’s harder to generate enough pressure to stop the flow of urine
- Things get hot, hot, hot, especially at night. Hot flashes occur commonly as a result of these hormonal changes and can disrupt sleep.
- Blood flow (and lubrication) to the vulvar tissues decreases, which can make it harder to achieve an orgasm. Incidence of anorgasmia is increased in post-menopausal people.
- This intense hormonal shift, combined with lack of sleep, can lead to mood changes or depression. The incidence of depression is 2- to 5-fold higher in perimenopause compared to late pre-menopause.
How sex changes
In short, you’ve got less vulvar tissue to work with, so sex can get uncomfortable. It’s a combination of decreased blood to the genitals, thinning of the tissue, shrinking of the muscles, plus changes in libido for some folks. Common complaints are reduced sexual desire, vaginal dryness, dyspareunia (pain during sex), and difficulty achieving orgasm, but how ‘common’ these issues actually are is difficult to pin down. This is partially because study sample size, design and hormonal status are variable across research studies. One study found that prevalence of sexual dysfunction increased from 42% to 88% from early to late menopausal transition. It also may be hard to get clear statistics because most of these studies reference cis-gendered women, and may miss folks who retain a uterus and ovaries but do not identify as female. A person’s libido can change as well, and while it would be so simple to chalk up a change in libido in menopause to decreasing estrogen levels alone, it’s not that simple. Libido is complex with a lot of variables involved, including “biological, psychosexual, sociocultural and context-related factors”. There’s several other things that happen concurrently with menopause, and it can be difficult to untangle the affects of these events from strict physical changes in the body. This can include things like marital conflict, parental roles shifting as children move out of the house, and increasing rates of other diseases. If someone is partnered and that partner has a penis, erectile dysfunction rates also increase with increasing age (and concurrently with other diagnoses like diabetes or cardiovascular conditions), which can also play a role in your libido.
What about hormone replacement therapy (HRT)?
This is a tricky and hotly debated topic, with some things we do know and others that we don’t. Hormone replacement therapy is supplying the body with estrogen in one of two forms- systemically, like in the form of a pill or patch, or locally, like in the form of a low-dose cream applied to the vulva and vagina. What we do know is that supplemental estrogen is not processed by the body in the same way that estrogen produced in the body is, despite being chemically similar. What we don’t know is if oral HRT increases someone’s risk of cardiovascular disease, and how that varies with dosage, other health problems or when someone starts taking HRT. Estrogen produced in the body appears to protect the heart prior to menopause, because vagina-owners have lower rates of cardiovascular disease compared to age-matched penis-owners- but this changes dramatically with menopause. Oral HRT does not appear to protect the heart in the same way. Local creams have local effects: estrogen vaginal cream has better evidence than oral estrogen therapy for improving vaginal dryness and dyspareunia, but this doesn’t directly influence sexual frequency or low libido.
How to move forward
The way that menopause affects the body and sex will look at a little different for everyone. On the plus side, menopause occuring at midlife may coincide with events like retirement or becoming empty-nesters, which may lead to more freedom surrounding sex. Interventions that can alleviate the effects of menopause focus on improving blood flow (systemically and to the genitals), taking care of your mental health, improving lubrication
- Move. Your. Body! As we get older, a sedentary lifestyle is notorious for causing all sorts of unwanted effects, including decreased blood flow- which includes the vulvar tissues, too. Aerobic exercise improves elasticity of your arteries which means improved blood flow. More blood flow, easier to engorge vulvar tissues equals more sensation and more pleasure.
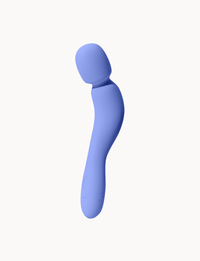
- IYKYK, Dame makes some amazing vibrators can get blood flow to the genitals more quickly.
- A sex therapist can help navigate changing roles and desires from a cognitive standpoint, because it’s so much more than physical changes that can impact how sex fits into your life post-menopause.
- A high-quality lube can help alleviate vaginal dryness.
- Hormone replacement therapy may be appropriate in some cases, like if vaginal dryness or tissue thinning are the main factors that’s stopping you from having sex, but this is at the discretion of a prescribing medical professional.
Menopause doesn’t have to mean sex is out of the question. Some modifications may be necessary, but the more knowledge you have, the easier it is to navigate this transition period.